Awake, Walking, and Intubated – The ICU Breakthrough Giving Patients Their Lives Back
“If they knew what it’s like for patients surviving after the ICU, that sedation isn’t sleep, and that they’re being so traumatized and damaged by these normal practices, they would change this.”
Picture this: it’s your first shift in the ICU as a new nurse and you walk in, expecting to hear nothing more than the blips and beeps of the machines keeping your silent and sedated patients alive—only to find patients on full mechanical ventilation, fully awake, alert, and taking a stroll with their family member.
No, you didn’t travel to an alternative reality, but it is a reality that supporters of the Awake and Walking ICU movement like Kali Dayton (@daytonicuconsulting), DNP, AGACNP, critical care nurse practitioner, host of the Walking Home From The ICU and Walking You Through The ICU podcasts, and critical care outcomes consultant, are hoping to make a new normal. Awake and Walking ICUs are exactly what they sound like—they are ICUs where medical staff care for critically ill patients, but they do it in a revolutionary way that focuses on minimizing deep sedation and prioritizing early mobility.
“An Awake and Walking ICU is an ICU that has mastered the ABCDEF bundle, meaning that they only use continuous sedation when there is an actual medical indication for sedation,” Dayon explains. “When there is an indication for sedation—an absolute need for it—then the safest sedative is given at the lowest dose for the shortest duration. So really, we’re trying to avoid or minimize sedation, implement safe sedation practices, and ensure patients are doing their highest level of mobility (unless there’s a contraindication to mobility) shortly after admission to the ICU, along with open family visitation.”
Dayton founded Dayton ICU Consulting, a company that trains hospitals to convert traditional ICUs into Awake and Walking ICUs, which are associated with significantly better outcomes for patients, lower costs for hospitals, and decreased workload and risks for nurses and staff. ICUs across the country are slowly adopting the methods into practice, such as Johns Hopkins, which implemented the concept in their adult ICUs and a PICU UP! Early Pediatric Mobility program in their pediatric ICUs.
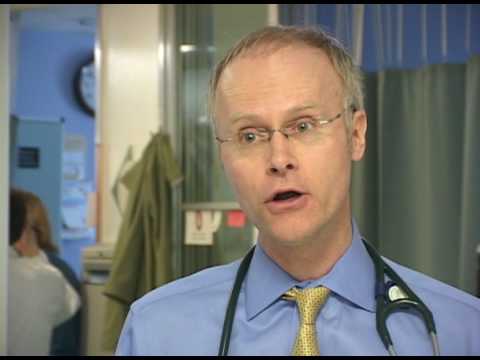
YouTube Video from John Hopkins on the Awake and Walking ICU from 15 years ago!
As Dayton describes it, the work she does is a “revolution,” so if you’re ready to have everything you thought you knew about ICU care flipped completely upside down, read on for Nurse.org’s exclusive interview and why she believes standardized Awake and Walking ICUs are the future of critical care.
Awake and Walking ICUs exist thanks to the pioneering efforts of Registered Nurse Polly Bailey, a shock trauma ICU nurse in Utah during the 1990s, who questioned the system of leaving patients deeply sedated and immobilized. After speaking to a young mother in her 30s who survived a weeks-long stay in the ICU following a battle with acute respiratory distress syndrome (ARDS), Bailey witnessed firsthand the profound physical and psychological trauma the patient had as a result of the standard care practices she had undergone in the ICU, including bedrest and deep sedation.
Bailey realized that change was necessary, so she worked with her ICU’s medical director
Dr. Terry Clemmer to begin reducing sedation and mobilizing intubated patients—to great success. Eventually, Bailey was able to do the training for a brand-new respiratory ICU and teach a new set of former long-term nurses who had no preconceived notions about ICU care on her new “Bailey Method” of waking patients up almost immediately after intubation and teaching them to cope and move to preserve muscle function while still ventilated.
Eventually, fellow nurses, especially Louise Bezdjian—who initially was a skeptic of Bailey’s methods until she saw the immediate and long-term benefits to ICU patients and survivors—an APRN who continues to work as a nurse practitioner and advocate for Awake and Walking ICUs. The two would publish their findings in a first-of-its-kind study in 2007, demonstrating that early activity is both feasible and functional in respiratory failure patients.
Not only did they prove that mobility was possible on mechanical ventilation, but their methods and research showed that keeping patients up and active helped solve the severe muscle atrophy and wasting in the ICU that leads to even more severe complications. Even when patients are healthy enough to be taken off the ventilator, weeks or months of sedation can make them too weak to recover properly and create a whole new set of complications like pressure sores, weakness and falls, and infections.
If you’re having a difficult time imagining how on earth a sedated patient—often associated with the image of someone coming out of it swinging and raring to yank out their own tubes—Dayton says you’ve got it all wrong. The reason the healthcare world has that image of a patient is precisely because of the time a patient has been under deep sedation. If you take a patient who’s been under deep sedation on a ventilator for weeks or months and suddenly decrease their sedation, they will be so confused and traumatized, that the natural reaction is severe confusion and agitation, Dayton explains.
Bailey’s methods, on the other hand, focus on reducing sedation as much as possible, as soon as possible after intubation so the patient is aware and able to participate in their plan of care. According to Dayton, this helps patients understand what’s happening, so they’re not confused and agitated, will not pull at their tubes, and can communicate when they are in discomfort so pain can be adequately controlled.
“We’re working towards having patients awake right away, informed, strong and confidently intact, to communicate their needs, understand their tubes, be calm and be able to mobilize promptly,” Dayton explains.
Bailey’s early methods would later be further backed by the Society of Critical Care Medicine’s ABCDEF Bundle, introduced in 2014, to reduce death, delirium, and hospital readmissions:
- A Element: Assess, Prevent, and Manage Pain
- B Element: Both Spontaneous Awakening Trials (SATs) and Spontaneous Breathing Trials (SBTs)
- C Element: Choice of Analgesia and Sedation
- D Element: Delirium: Assess, Prevent, and Manage
- E Element: Early Mobility and Exercise
- F Element: Family Engagement and Empowerment
Today, Dayton is working to implement the ABCDEF bundle by spreading Bailey and Bezdjian’s work and mission of converting traditional ICUs into Awake and Walking ICUs.
Dayton is a rarity in the ICU nursing world because her first job as a critical care nurse was in an Awake and Walking ICU, so the “normal” nursing care she learned as an ICU nurse included mechanically ventilated patients awake and moving around regularly.
“They treated having patients awake and walking even while intubated as routine and normal as giving an antibiotic,” Dayton recalls. “I didn’t know anything else.”
Dayton adds that she “hardly even knew how to titrate propofol” because it was so normal to have ventilated patients writing on a clipboard and completely awake off of all sedation. So when she became a travel nurse and worked in a more traditional ICU setting, she was shocked to find that all patients on ventilators were automatically sedated.
“When I tried to explain what I was used to and why I was confused and concerned about this, everyone thought I was crazy,” she says.
Eventually, Dayton returned to her original Awake and Walking ICU and enrolled in graduate school. But after being a travel nurse for years, her re-entry into the world of non-sedated patients on ventilators felt like a shock to the system yet again.
“I was almost shocked again to see really sick patients—patients with ARDS, septic shock, multi-organ failure, BMT patients—awake and walking, and then they walk out the doors…this is so different than what I just spent my time doing the last two years,” she notes.
The problem, Dayton soon realized, was that while she had been trained on the practices of mobile sedation, she hadn’t learned the why behind them. Fortunately for her, she worked for Bailey and Bezdjian, the very nurses who had worked to implement lowered sedation and mobility practices in the ICU, so she was able to learn from them and dig into the research backing the movement.
“I was like, why are we the only ones to do this here?” Dayton recalls. “I ran into survivors, and as I was putting all these pieces together, I just kept thinking, ‘The ICU community doesn’t know this.’ If they knew what it’s like for patients surviving after the ICU, that sedation isn’t sleep, and that they’re being so traumatized and damaged by these normal practices, they would change this.”
Dayton’s desire to change the culture around critical care was born and she started her Walking Home From the ICU podcast, where she interviewed ICU survivors and colleagues who helped her explain the research and evidence-based practices behind Awake ICUs. During her time of advocacy, she soon realized the need for hospitals to have resources to transform their own ICUs, so she developed Dayton ICU consulting, which does just that, with education and hands-on training to implement Awake and Walking ICUs.
As Dayton explains to both those who consult with her and those just interested in learning more, the methods behind Awake and Walking ICUs are researched-backed and evidence-based. And the numbers are startling and speak for themselves.
According to Dayton, some of the statistics about the practices behind Awake and Walking ICUs include:
- 60% less physical restraints when minimal to no sedation is used
- Decreases seven-day mortality by 68%
- Decreases delirium by 50%
- Decreases readmission to the hospital by 46%
- Decreases discharges to anywhere but home by 36%
- Decreased time on the ventilator
- Decreased time in the hospital
In contrast, traditional ICUs, with deep sedation are associated with statistics such as:
Despite the research and statistics, Dayton notes that the reluctance to adopt Awake and Walking ICUs stems from many factors, including a lack of knowledge about the dangers and experience of ICU patients, unfavorable experiences medical professionals have had trying to take a deeply-sedation patient off sedation, as well as she calls a “malignant normalcy” of the overarching culture of ICU care.
She adds that both nurses who have worked ICU for years as well as newer nurses who entered critical care during the COVID-19 pandemic have learned a model of “sedation and mobility.”
“It’s just so normal, it’s a routine, it’s a conveyor belt, they know what to do,” she says. “So it’s about getting them to stop and question, are we really practicing evidence-based medicine?”
One of the main principles that Dayton educates nurses and other medical professionals on in her work is the misconception that sleep = sedation.
She explains that many sedation medications, including both benzodiazepines and propofol, prevent REM sleep stages 3 and 4 from occurring in the brain. Without the REM cycle completed, sleep cannot physically happen in the brain. Deep sedation can have outcomes in line with sleep deprivation, including hallucinations, depression, cognitive impairment, PTSD, and even death.
“You can come in with pneumonia and leave with a new brain injury that’s like mild Alzheimer’s or a traumatic brain injury, as well as a new neuromuscular condition, just because you had pneumonia,” Dayton notes.
As part of her podcast, Dayton also shares the stories of ICU survivors, who recount their own traumatic experiences with deep sedation. A common theme she says she sees among survivors is that because the brain is not biologically asleep yet can also not function enough for communication, patients on deep sedation may experience the brain trying to make sense of what is happening—a process that can, unfortunately, lead to trauma.
For instance, one survivor was so traumatized by her experience under sedation that she drafted a document with an attorney to avoid it happening again to her. When she developed another respiratory condition, she was able to be treated in an Awake and Walking ICU where she explained that she “wasn’t afraid of the ventilator, just sedation.”
Another survivor who experienced a severe fever while under deep sedation was treated with cooling bags and believed that she was on ice because doctors were preparing to harvest her organs.
“A lot of it’s rooted in what they’re actually experiencing, but they are not allowed to actually be informed and be in reality,” Dayton explains. “So they find a real way to understand why they’re in pain, why their body’s stressed, and most survivors I’ve talked to say, ‘I would have so much rather have been was in the ICU than where I was in my mind.'”
If you’re reading this with a face of horror, it’s probably mirroring the exact face I had when interviewing Dayton. My thoughts floated to the few times I had floated to ICU as a new nurse—did I cause harm to my patients during the dark and almost eerily silent nights I had spent there?
Dayton, however, is quick to assure me—and all nurses—that while it can be normal to feel some guilt in seeing sedation and typical ICU care in a new light, she wants nurses to feel empowered, not overwhelmed.
“My hope is that nurses realize that none of this is their fault, they were born into this,” she points out. “But I want to leave with hope that the burdens we’re suffering from so severely right now don’t have to be the standard. We can make a change and a difference.”
She encourages any current or prospective ICU nurse to do more research on Awake and Walking ICUs, listen to her podcast for even more compelling evidence and stories, and talk to their executive leadership about strategies that can be implemented.
She also points out that there are practices and tools that any ICU nurse can enact right now, such as upright beds to reduce pressure, being diligent about assessing Richmond Agitation-Sedation (RAS) scores, and advocating for patients to have decreased sedation, as light sedation—not deep sedation—is the target for mechanical ventilation, even with severe ARDS.
Dayton also wants nurses to know that the standard practices of deep sedation can create much more work for them when it is time to bring the patient out of the sedated state.
“It’s important to recognize that nurses are the biggest victims of this, second only to patients and families,” she explains.
“Nurses are the ones that have to deal with the confused patients trying to hit them, assault them, climb out of bed, pull out their lines and tubes,” she continues, adding that delirium doubles the nursing hours required for care. “It increases time in the ICU by almost five days and overall time in the hospital by almost seven days, and those are not pleasant extra days,” she adds.
Implementing the ABCDEF Bundle with an Awake and Walking ICU, Dayton explains, makes many of the hurdles of post-sedation care much easier. For instance, instead of needing 5 people to move a weak patient who’s been on a vent and in deep sedation for two weeks and is now a severe fall risk, it could take only one or two to mobilize a patient shortly after intubation.
“It’s easier to move patients, it’s easier to talk to them, to de-escalate things, to manage their pain,” she notes. “All these things are so much easier than trying to wrangle someone that’s confused and trying to pull everything out or hit them. What’s in it for the nurses is greater career fulfillment, more safety, and an easier workload, even though it goes against anything that they would initially perceive, right?”
Dayton fully believes that Awake and Walking ICUS will become the standard model of care, with medically induced comas serving as exceptions only when truly medically indicated.
“Everyone needs to understand the why and the how of what we’ve missed for so many years and until we are more afraid of delirium and ICU-accrued weakness than self-extubation, we’ll never get there,” she says. Due to the hurdles of changing culture, she adds that it will most likely be a long road ahead.
“I think for the next number of years, it’s going to be one ICU at a time,” Dayton says. But still, she is hopeful and notes that she already has trained 13 hospitals to implement Awake and Walking ICUs across the country, including in Denver, Colorado area, Sacramento, Seattle, Bellingham, Washington, Kentucky, and an ongoing development in Grand Rapids, Michigan.
“I think one nurse can make a difference for one patient at a time…and then once it gets rolling and self-sustaining, it will be easier and everyone’s like, ‘Oh, this is so much better, let’s never go back to that,'” Dayton says.
All images courtesy of Kali Dayton.