Care home staff describe ‘traumatic’ Covid experiences

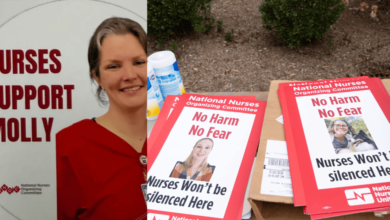
Traumatised nurses and other care home staff were afraid for the safety of the people in their care during the early stage of the Covid-19 pandemic, a new study has found.
Between 2 March and 12 June 2020, more than 66,000 care home residents in England and Wales died. Nearly 30% of these deaths were attributed to Covid-19.
“It was just a horrible, horrible time”
Care home manager
Researchers at Northumbria University interviewed 70 care home staff and healthcare professionals involved in the transition of care between hospitals and care homes during the pandemic to find out about their experiences during this period. These interviews were carried out between January and October 2021.
The results, published in the journal Age and Ageing, showed that in the early stages of the pandemic, care home staff felt under pressure to receive patients discharged from hospital, even when the patient’s Covid-19 status was unclear.
One care home senior manager told the researchers that “hospitals just wanted patients out, regardless of Covid status”. They added: “In those early days, you know, it was very traumatic.”
Care home staff expressed fear, anxiety and emotional stress from working during the pandemic.
A care home local manager said in their interview: “It was just a horrible, horrible time, and you just didn’t know what staff member next was going to be positive, because obviously if they’re positive they can’t come in.”
The interview participants also expressed fear for the safety of the care home residents, due to the high risk of infection caused by inadequate Covid-19 testing and poor infection risk communication.
A care home local manager said in an interview: “We had a phone call from a nurse from the hospital to say that ‘… this lady was lying beside somebody, less than two meters, who was Covid positive.’
“So straight after that call we did an LFD test and it was positive and Covid spread through our home like wildfire.
“It was the most horrendous time. I never want to go through that ever again. It was horrendous. We lost seven clients to Covid.”
The researchers also found that care home staff felt the protocols put in place to reduce the spread of Covid-19 resulted in “dehumanisation”, with the degree of isolation experienced by care home residents in many cases hard to endure.
The practice of taking someone from hospital to a care home without permitting any social contact was likened to treating care home residents as prisoners. As one paramedic told the researchers: “They’re not prisoners, we were treating like they were because we effectively put them in a cell. My job was made difficult from a care perspective.”
However, the researchers also found that the changes made to adapt to Covid-19 restrictions resulted in better ways of working in some cases. These included improved infection control, better working relationships and improved integration and access with health services, with the move to remote access through digital technologies.
Associate professor of health and social care quality at Northumbria University, Dr Jason Scott, told Nursing Times: “There were certainly some huge areas for improvement and a lot of things that did not go well during transitions during Covid, particularly around the lockdowns.
“Some of those problems came to the forefront during the pandemic because they could no longer be masked”
Jason Scott
“The care homes were in this situation of being responsive to the policy that was shifting week to week. They had to develop new ways of working.”
Dr Scott said he hoped the research would “shine a light” on the issues raised by participants, and lead to a better alignment of health and social care.
He said: “If something goes wrong in health care, there are more robust mechanisms in place to learn, but it’s very different in social care, where there’s often a ‘fix and forget’ approach to problems that occur when people transition between services.
“That approach stops problems taking up more resources and means they’re often masked from residents because they are fixed before they can cause worry or distress.
“But it means the sector is limited in its ability to learn or influence change, and so the same problems can happen repeatedly.
“Some of those problems came to the forefront during the pandemic because they could no longer be masked.
“Before then, transitions from hospitals to care homes would not have received media attention, they wouldn’t have made for a big national story – but then suddenly, they did.”
Module 6 of the UK Covid-19 inquiry opened in December 2023 and is dedicated to investigating the impact of the pandemic on adult social care in England, Scotland Wales and Northern Ireland.
Preliminary hearings are scheduled to take place in early 2024 in London and will be open to the public.