End-of-life care planning ‘needs to become routine’

Nurses need to support a “culture change” in end-of-life care whereby people’s wishes are better recorded and respected, a new report has urged.
The report, by Compassion in Dying, is based on analysis of 5,000 calls and emails to the charity’s nurse-led helpline as well as new polling of the public by YouGov.
“Our code as nurses clearly states that we need to act in the best interests of the people we’re looking after at all times”
Sarah Malik
The findings showed that not enough people were being supported to make advance decisions about their care at the end of life.
In situations where people had recorded their preferences and had opted to refuse treatments, these wishes were not always being respected by health professionals.
The report also warned that some people were not being provided with honest information about their prognosis, making it difficult for them to make informed decisions about their care.
“Some people are not told they are dying even when they ask,” stated the report, titled Rethinking the UK’s approach to dying – Lessons from an end-of-life helpline.
“Others are told critical information about their treatment options or prognosis in euphemisms or with terminology they do not understand.”
The report made a number of recommendations which the charity hoped would lead to a new culture within healthcare and society in which end-of-life conversations were normal and routine.
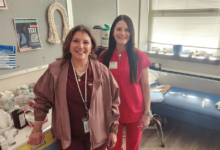
Sarah Malik, clinical lead and services manager at Compassion in Dying, heads up the charity’s nurse-led helpline, and is a nurse herself.

Sarah Malik
She said failures in recording or respecting advance decisions meant “people end up subjected to ambulance rides they wanted to avoid, undergoing hospital admissions against their wishes, or receiving treatment they would not have wanted”.
“Our code as nurses clearly states that we need to act in the best interests of the people we’re looking after at all times, balancing that with the requirement to respect a person’s right to accept or refuse treatment,” Ms Malik told Nursing Times.
“But what I’m hearing sadly shows that too often, this just isn’t happening.”
She said nurses should be the “champions of patient choice and autonomy”, but that they needed training and support to raise their confidence in seeking and respecting people’s wishes.
“Instilling the recommendations of this report will help us all to improve people’s end-of-life experience, putting them back at the centre of decision making,” added Ms Malik.
Among the recommendations was for the introduction of a new “guarantee” that everyone will be offered the chance to make an advanced care plan.
The report suggested that advance care planning conversations should be incorporated into the NHS health check at certain ages and revisited over time.
To raise awareness among the public about advance care planning, the report also recommended that a new public health campaign on this topic should take place.
In addition, it called for mandatory training to be introduced for health professionals on end-of-life care decision making.
The charity also wanted to see a new “duty of openness and transparency” for end-of-life care conversations to ensure people were able to give properly informed consent for treatments.