Harms from NSAIDs scripts in high-risk groups costing NHS millions
Prescribing non-steroidal anti-inflammatory drugs (NSAIDs) to patients at high risk of harm from them is estimated to cost the NHS in England around £31m a decade, according to a study findings.
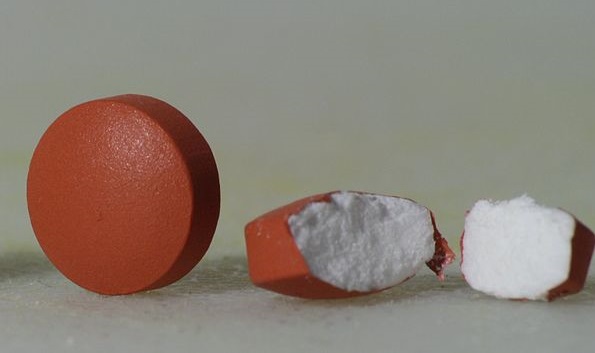
Researchers noted that NSAIDs were one of the most widely prescribed drug types globally, but were known to increase the risk of gastrointestinal bleeding, heart attacks, stroke and kidney damage.
“In practice, reducing NSAID prescribing on an individual level by prescribers is challenging”
Study authors
But they stressed that NSAIDs continued to be a source of avoidable harm and healthcare costs, and more needed to be done to address this challenge, especially among high-risk patient groups.
Prescribing was still common in groups defined as such due to older age, previous peptic ulcer, heart failure, chronic kidney disease, or who are taking other medications that can increase bleeding risk.
As a result, the researchers set out to estimate levels of patient harm and the costs of NSAID prescribing to high-risk groups in the NHS in England over a 10-year period.
The study, funded by the National Institute of Health and Care Research, involved the University of Manchester, University of Nottingham, University of Edinburgh and University of Southern Denmark.
Researchers drew on previously published research on prescribing safety in England, which provided a baseline number of patients affected by so-called ‘hazardous prescribing events’ in April 2020.
The data came from 1,060 GP practices in England and involved 10,906,453 patients in total, noted the researchers in the British Medical Journal.
They identified hazardous prescribing events for oral NSAIDs in five high-risk groups – adults aged 65 and over with no gastroprotection, those with a previous peptic ulcer and no gastroprotection; those concurrently taking anticoagulants; heart failure patients and chronic kidney disease (CKD) patients.
The researchers estimated the harm associated with each event, expressed as quality adjusted life years (QALYs) lost – a measure of years lived in good health – and NHS costs in managing that harm.
Results showed average QALYs per person – where 1 is equivalent to perfect health and 0 represents being dead – were between 0.01 lower with previous peptic ulcer to 0.11 lower with CKD.
Average costs increased from a non-statistically significant £14 in heart failure to a statistically significant £1,097 in people also taking anticoagulants, said the researchers.
In addition, they found rates of hazardous prescribing events per 1,000 patients ranged from 0.11 in people with a previous peptic ulcer, to 1.70 in older adults.
Nationally, the most common event – older adults without gastroprotection – resulted in 1,929 QALYs lost, while the greatest impact was in those also taking anticoagulants, with 2,143 QALYs lost.
Over 10 years, the five NSAID related hazardous prescribing events led to a total loss of 6,335 QALYs at an estimated cost of £31.43m to the NHS in England, according to the study authors.
Shorter durations of exposure were associated with lower risk of harms, but at least half of the observed harms occurred in the first 1.5 years of treatment, the authors noted.
Writing in the BMJ, they stated: “NSAIDs continue to be a source of avoidable harm and healthcare costs, despite a range of initiatives to reduce their use, especially in populations at high risk.
“The risk of harm and associated costs appear to outweigh their benefit in these populations; therefore, a concerted effort should be made to continue to include NSAIDs in patient safety and deprescribing initiatives.”
They added: “The key implication for policy and practice is that, despite quite large improvements in high risk prescribing of NSAIDs in the past 10-15 years, more work needs to be done.
“In practice, reducing NSAID prescribing on an individual level by prescribers is challenging because it depends on how much pain a patient is in, how well they respond to NSAIDs, and how well they respond to other analgesics or interventions.”






