Intermittent Fasting Diet Plan
Obesity is a well-known worldwide epidemic that is a risk factor for developing heart disease, diabetes, certain types of cancer, and many other health issues. As the obesity epidemic continues, people have developed interest for weight loss programs and diets. Nurses are often sought after by family, friends, and peers for expert opinion on all things related to health, including diet. Intermittent fasting is one of the many diet trends circulating around conversations and diet internet searches, so here’s what nurses need to know.
Types of Intermittent Fasting (Patterson, et al., 2016)
Intermittent fasting involves the restriction of eating or caloric intake at intermittent intervals. The literature mentions three methods to achieve this, including alternate day fasting, time-restricted feeding, and modified fasting regimens.
Alternative day fasting involves not consuming food for an entire day alternating with days where food and drink are consumed ad libitum. For example, a person may eat at will for three days, fast for one day, then eat at will for two days, and fast the following day.
Time-restricted feeding is defined as eating foods within a designated period, then fasting for the remaining hours of the day. There are various fasting intervals mentioned in the literature ranging from twelve to twenty hours, but for example, a person may consume food during an eight-hour period, then fast for the remaining 16 hours of the day. Or a twelve hour fast could be as simple as not eating after a 6 pm dinner until waking at 6 am then next day.
Modified fasting regimens is the basis for the popular 5:2 diet which involves consuming 20-25% of energy needs on fasting days on two non-consecutive days of the week and eating ad libitum the other five days.
While people following a fasting plan can eat “at will” during non-fasting times, it is suggested that the food choices be healthy. To avoid dehydration during fasting intervals, water and unsweetened coffee and/or tea should be consumed.
The Science Behind Intermittent Fasting (Tello, 2018)
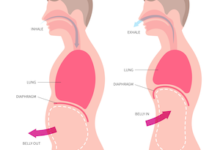
Intuitively, intermittent fasting makes sense that by restricting eating times, you would overall intake less calories, and therefore lose body weight, but what is the science behind this on a cellular level? Let me explain. Food is our bodies fuel, so the food we eat is broken down in our gut and eventually becomes molecules in our circulation available as an energy source by our cells. Carbohydrates are rapidly broken down into sugar (glucose) but if these molecules are not used for energy, insulin is secreted by the pancreas to transport the sugar into fat cells for storage. When we have periods of fasting, even short ones like abstaining from snacking between meals, insulin levels decrease because there are no sugar molecules that need cellular transport. The fat cells then release stored sugar to use as energy (ketosis). More simply, we lose weight during fasting as a result of low insulin levels that signal the body to burn off fat for energy.
Health Benefits
There is research on human subjects complying with various intermittent fasting diet plans, with and without the addition of an exercise plan, that have looked not only at weight loss benefits but other biomarkers. Some researchers believe that intermittent fasting regimens where the last meal is consumed early in the day, may leverage the circadian biology to improve overall metabolic health. Desynchronization of circadian rhythms can lead to chronic diseases such as obesity, diabetes, cardiovascular disease, and certain types of cancer. Gastrointestinal microbiota and gut function are also closely related to circadian rhythm. Gastric emptying/blood flow and metabolic responses to glucose load are quicker in the morning than in the evening. Some researchers believe intermittent fasting may directly positively influence gut microbiota (Patterson, et al., 2016).
For example, a study conducted in 2018 by Sutton, et al., included pre-diabetic men with a control group who had a 12-hour eating period and study group who had 6-hours eating period where last meal was consumed by 3 pm. The results showed the study group had improved insulin sensitivity, blood pressure, oxidative stress, beta cell responsiveness and appetite, surprisingly even without significant weight loss (Sutton, et al., 2018).
In 2016, Patterson, et al., analyzed several studies on humans on an intermittent fasting plan. They found statistically significant weight loss on 85% of the trials as well as appetite-regulating hormone levels. They also noted that numerous studies have reported an association between nighttime eating and reduced sleep duration and poor sleep quality. They hypothesized that eating at abnormal circadian times leads to overall circadian desynchronization.
Finally, researchers at Johns Hopkins School of Medicine are studying the effects of intermittent fasting and brain function. The results so far have been positive. They have reported that even fasting two days a week can improve neural connections in the hippocampus and protect the neurons from accumulating amyloid plaques, which is a protein prevalent in Alzheimer patients. Also, ketones (created by ketosis) promote positive changes in the structures of the synapses. They claim fasting challenges your brain in a healthy way that can ward off neurodegenerative diseases, such as Alzheimer’s and Parkinson’s. The researchers state that when your brain is challenged, whether it be by exercise, cognitive tasks, or fasting, the body produces a protein call brain-derived neurotrophic factor (BDNF) that strengthens neural connections, increases production of new neurons, and can have an anti-depressant effect (Sugarman, 2016).
There is still a lot of research to be done on intermittent fasting, as well as other diet plans, but with the obesity epidemic and prevalence of chronic diseases, the work will undoubtedly continue. The research is quick to point out that while there is a lot of positive information about intermittent fasting it is not appropriate for individuals who have type 1 diabetes, are pregnant or breastfeeding, the elderly, or people who have history of eating disorders (Ganesan, et al., 2018).
References:
Ganesan, K., Habboush, Y., and Sultan, S. (2018). Intermittent fasting: The choice for a healthier lifestyle. Cureus,10(7): e2947. doi: 10.7759/cureus.2947
Patterson, R. E., Laughlin, G. A., Sears, D. D., LaCroix, A. Z., Marinac, C., Gallo, L.C….Villaseanor, A. (2016). Intermittent fasting and human metabolic health. Journal of the Academy of Nutrition and Dietetics, 115(8): 1203–1212. doi: 10.1016/j.jand.2015.02.018
Sugarman, J. (2016). Are there any proven benefits to fasting? Retrieved from https://www.johnshopkinshealthreview.com/issues/spring-summer-2016/articles/are-there-any-proven-benefits-to-fasting
Sutton, E. F., Beyl, R., Early, K. S., Cefalu, W. T., Ravussin, E., and Peterson, C. M. (2018). Cellular Metabolism, 27(6), 1212-1221.e3. doi: 10.1016/j.cmet.2018.04.010
Tello, M. (2018, June). Intermittent fasting: Surprising update. Retrieved from https://www.health.harvard.edu/blog/intermittent-fasting-surprising-update-2018062914156
Volpe, S.L. (2019). Intermittent fasting- what is it and does it work? American College of Sports Medicine, 23(1), 34-36. doi: 10.1249/FIT.0000000000000444