Report: Future Nurse roundtable on remote care


In November 2023, Future Nurse convened a roundtable of senior nurse leaders to discuss the hot topic of virtual wards.
Each individually selected participant came equipped with a wealth of experience in remote care and digital transformation ready to share insights gained from innovating on the frontline of health and social care.
An agenda had been set for the afternoon to cover a breadth of topics to uncover how nursing is evolving to incorporate tech enabled care at home, wherever home is for the patient.
Discussion centred on three key areas designed to develop a deeper understanding of this evolution and different approaches to tech enabled remote care, the impact of the acceleration of these ways of delivering care for the nursing workforce and the professional leadership needed to shape the future of person-centred care enabled by technology.
Questions for discussion
Where can technology best support – person-centred, place-based care and population health? How is it used, what is needed and where do we see the most value?
Workforce for the future – will new ways of working positively impact our recruitment and retention challenge?
Leadership – what is the leadership role of nurses in designing and delivering virtual wards and other remote care models?

The panel
Chair: Natasha Phillips, founder of Future Nurse and former national chief nursing information officer at NHS England
Rebecca Ashworth, lead nurse for clinical engagement/clinical safety officer, Doccla
Rachel Binks, nurse consultant and clinical lead for digital care hub, Airedale NHS Foundation Trust
Mark Goodfellow, digital clinical lead (virtual ward), Shropshire Community Health NHS Trust
Hayley Grafton, chief nursing information officer, University Hospitals of Leicester NHS Trust
Zoe Harris, chief nursing information officer, Nottingham University Hospitals NHS Trust
Fiona Hibberts, head of the Nightingale Academy and consultant nurse, Guy’s and St Thomas’ NHS Foundation Trust
Claire Madon, chief nursing information officer, Sherwood Forest Hospitals NHS Foundation Trust, and CNIO for Midlands Region, NHS England
Sam Neville, chief nursing information officer/clinical safety officer, Mid and South Essex NHS Foundation Trust, and CNIO for Eastern Region, NHS England
Multiplicity of approaches: Amidst their experiences, the participants noted the rapid evolution of remote care practices, underscored by technological advancements that have redefined the landscape. All highlighted the need for a shift from focusing on early discharge to long term condition management.
An exploration of the myriad approaches to remote care, recognised the diversity of telehealth and remote care solutions in nursing practice.
The group’s experience went back to 2011, echoing the broader trend in nursing and reflecting the integral role telehealth and remote monitoring has played in long term conditions management.
All agreed this is not new, although virtual wards have been conceptualised as new and the defining features of this model that made them different to what has gone before were teased out.
Positive Impact of technology: All emphasised the positive impact of technology during the pandemic and the shift in perspectives of health care professionals and patients who now seem to recognise the value of virtual care in ensuring healthcare continuity.
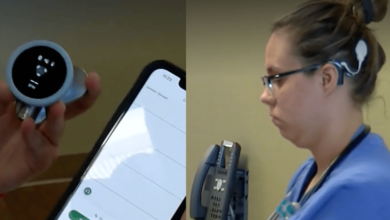
Vision for the future: The seasoned leaders shared their vision for the future, expecting an expansion of the integration of innovative technologies like artificial intelligence and wearable devices into the fabric of nursing practices.
These would enable more and higher quality models where remote monitoring and support become an integral part of the pathways of care for increasing numbers of patients.
The conversation moved from the what to the how and specifically the changing nature of the work and the needs of the workforce to practice in new ways whilst maintaining the ethos of nursing practice.
This included what it is to be a nurse and the unique contribution of nurses in making a success of remote care. We were reminded of the professional focus on wellbeing and independence with Virginia Henderson’s definition of nursing quoted:
“The unique function of the nurse is to assist the individual, sick or well, in the performance of those activities contributing to health or its recovery (or to peaceful death) that he would perform unaided if he had the necessary strength, will or knowledge”
Connected care: the importance of staff staying connected with patients in their homes was highlighted, particularly during the pandemic, where virtual care emerged as a lifeline.
This led to a conversation where all were united on the need for person-centredness when developing and delivering remote care models.
Person-centred care: the participants all talked passionately about their experiences of leading remote care and the ways this was enabling truly person-centred care. They called out the following as key features:
- Continuous monitoring and early intervention: Aligned with the proactive management ethos of person-centred care, virtual wards enable continuous monitoring of vital signs and patient-reported data, facilitating timely interventions and adjustments to care plans.
- Empowering patients in self-management: Virtual wards serve as a conduit for patients to actively engage in their care by providing educational resources, self-monitoring tools, and real-time communication with healthcare professionals.
- Fostering therapeutic relationships: Through ongoing communication, virtual wards create opportunities for nurses to establish and nurture therapeutic relationships with patients, fostering trust, understanding, and partnership in the care process.
- Considering the whole person: Virtual wards incorporate comprehensive monitoring and diverse communication channels, allowing nurses to consider the whole person, including social determinants of health, mental well-being, and the patient’s daily life and routine.
The conversation moved onto the challenges of current approaches and where the best opportunities for improvement existed. This was grounded in the shared understanding of the intersection of person-centred care and technology that enables this to be delivered remotely that had been established.
Early discharge versus long-term condition management: The group acknowledged the success of virtual wards in facilitating early discharge, but participants emphasised the need to extend the scope beyond immediate post-discharge care.
The shift in focus needed is to leverage virtual care solutions that influence proactive management of long-term conditions, aligning with the broader goal of enhancing patient outcomes and quality of life.
Empowering self-management: Participants highlighted the potential of virtual wards in empowering patients to actively manage their long-term conditions. This involves providing tools, resources, and support mechanisms that enable patients to take control of their health journey.
The discussion emphasised the role of technology in facilitating health education, promoting lifestyle changes, and fostering a collaborative relationship between patients and healthcare providers.
Earlier admission avoidance: A key theme in the discussion was the proactive use of virtual wards to avoid unnecessary hospital admissions at an earlier stage of a patient’s condition.
By closely monitoring vital signs, symptoms, and adherence to care plans, healthcare providers can intervene pre-emptively, preventing exacerbations that might lead to hospitalisation.
The group recognized the potential cost savings and improved patient outcomes associated with a strategy focused on early intervention and admission avoidance.
Comprehensive, patient-centric care: The evolving concept of virtual wards encompasses a more comprehensive, patient-centric model of care.
This involves continuous monitoring, timely interventions, and personalized care plans tailored to the specific needs of individuals with long-term conditions.
The group discussed the importance of collaboration between healthcare professionals, patients, and support networks to ensure a holistic and effective approach to long-term condition management.
The conversation then moved to focus on the workforce and cultural challenges and what should be done to address these.
Cultural priorities: The group were passionate about the need to shift the focus of virtual wards in this way and highlighted some of the cultural changes needed to achieve it.
The leaders unanimously recognized the importance of breaking down organisational silos, fostering collaboration across departments and specialties for effective remote care.
Remote models of care like virtual wards can contribute to healthcare accessibility and equity by making high-quality nursing care accessible to individuals in remote and underserved areas.
All agreed that nurses had an important role to play in ensuring that this happens through use of tools like equality impact assessments and through engagement of and co-design with patients.
The leaders underscored the significance of trust in technology, acknowledging that fostering trust is a critical factor in promoting the benefits of remote monitoring.
All talked about the nurse patient relationship and our unique position as the most trusted professionals to support patients to trust the technology.
Workforce development priorities: The leaders acknowledged the imperative for nursing professionals to grow their digital literacy, increase their adaptability, and improve their advanced communication skills, a prerequisite for navigating the nuances of remote care.
The need for continuous education and professional development emerged as a central theme, emphasising the importance of staying abreast of the latest technological advancements through various training programs.
The participants recognised the collaborative efforts needed with educational institutions and healthcare organizations to mould a workforce adept at the intricacies of remote care.
Participants called for continuous learning and that the collaborative spirit of nursing communities has the potential to support not only adoption but learning and evolution of technology enabled models of remote monitoring and care.
The participants emphasised the potential societal benefits of data collaboration in healthcare and how it will help provide a comprehensive understanding of patient needs and outcomes.
They underscored the need for collaboration between acute and community care providers, ensuring seamless transitions and comprehensive patient care.
Many highlighted the importance of the effective use of dashboards for better visibility, enabling healthcare providers to make informed decisions based on real-time data.
All agreed that this is an area of professional immaturity and suggested nurses needed more training to ensure they had the data skills needed to effectively deliver and lead the changes.
The group were keen to call out the opportunities for addressing the recruitment and retention challenges faced by the profession:
Utilising technology for nurse retention: The potential of technology in retaining nursing staff by developing more remote care roles was explored.
Many reported that this way of working enhanced job satisfaction and provided avenues for professional growth. All agreed more should be done to expose student nurses to placements in remote care settings.
New roles: the discussion explored the creation of innovative roles in remote care, challenging traditional models and promoting inventive approaches to healthcare delivery.
There was collective excitement about the potential for new roles and new education opportunities.
Leading the agenda: challenges, opportunities and next steps
In the final roundtable theme, the group reflected on and summarised the conversation as it discussed the role of nursing leadership in shaping the future where technology enabled place-based person-centred care is a core part of nursing practice.
Honest conversations about risks: Participants believed it was vital that healthcare system was open about the risks and challenges associated with remote care, fostering transparency and shared learning.
Developing a remote care workforce: strategies for developing a remote care workforce, emphasising the cultivation of communication skills, adaptability, and continuous training.
Leadership community’s role: The influential role of senior nurse leaders in steering the direction of remote care became evident, with a call for advocacy at policy and practice levels.
Influencing policies and practices: Leaders shared their experience in shaping policies, practices, and vendor selections, reflecting a commitment to driving positive change.
Vision for the future
As the roundtable drew to a close, a shared vision for the future emerged – a future where technology enhances rather than hinders person-centred care.
The participants envisioned a healthcare landscape where innovation is a tool for delivering not just care but transformative, person-centred experiences that prioritise the unique needs and preferences of each individual. Specific areas of focus were:
- Person-centred care: Participants advocated for a shift to person-centred care and long term conditions management at place level
- Challenges in funding and virtual hubs: The participants discussed the challenges in funding virtual care initiatives and proposed the establishment of larger virtual hubs, addressing the need for centralised resources.
- Focus on research: The importance of research in advancing remote care practices emerged, with collaborative efforts between healthcare sectors contributing to evidence-based approaches.
Commitment to next steps: The commitment of the roundtable members to the next steps was clear and energising. There was a collective pledge to foster new connections, gain fresh insights, wield collective influence, and share their learnings beyond the group.
The aspiration was not merely to adapt to change but to actively shape the direction of virtual care towards a more compassionate, personalised future.
Closing Thoughts: In closing, the roundtable members expressed their shared dedication to advancing person-centred virtual care in the UK.
The transformative potential of technology was seen not as a departure from person-centred values but as an opportunity to deepen the personal connections between nurses and patients.
As the roundtable concluded, the vision for the future was clear – a future where healthcare is not only medically effective but deeply compassionate, personalised, and respectful of the diverse narratives that shape each person’s health journey.
The commitment of the roundtable members echoes the essence of nursing – a profession dedicated to caring for the whole person, in all their uniqueness and complexity, even in the virtual realm.
Thanks to Doccla for sponsoring this opportunity for a collective of experienced nurses leading remote care to come together to share experience, learn and debate next steps.