Nurses & Plantar Fasciitis: Keep Your Hard-Working Feet Healthy
Page reviewed and updated: August 2023
As nurses, we spend a lot of time on our feet. This holds true not only for bedside nurses but also for nurse educators, nurse practitioners and many, if not all, other nursing professionals. Our feet carry three times our body weight with each step. When you factor in the strenuous job duties required in nursing, i.e., lifting patients, lifting equipment, and running to a code blue, just to name a few, we add significant weight load on our feet. Furthermore, most of our walking and weight bearing at work is on hard surfaces – hospital floors and hallways, and the concrete stairs present in most healthcare facilities, which while providing a “sterile” environment, are unforgiving surfaces that do little to improve the shock absorption of our steps.
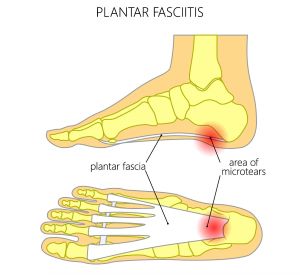
Plantar fasciitis is one of the most common causes of foot and heel pain in the United States. There are many risk factors associated with developing plantar fasciitis including obesity/high body mass index (BMI) in the non-athlete, running, and underlying structural deformities such as flat feet (pes planus), high arches (pes cavus), exaggerated pronation, or limited ankle dorsiflexion, but the condition is largely considered an overuse injury. While the precise etiology is not completely understood, it is thought to be due in part to microtrauma and inflammation from prolonged standing, walking, or running in conjunction with contributing risk factors noted above. Other factors include poor fitting or poorly supportive shoes and a recent increase in weight bearing activity (i.e., a new running or exercise program).
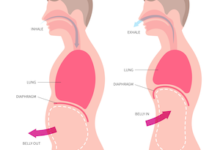
.jpg.aspx) Nurses are at high risk for developing plantar fasciitis due to our job responsibilities. The plantar fascia is composed of fibrous bands that insert at the heel (calcaneus) and connect to the toes (metatarsals). These bands provide support to the foot and in turn bear the weight of the body with ambulation and any weight bearing activity. The plantar fascia assists with shock absorption via a windlass mechanism. This refers to the fascia lengthening and increased tension on the medial longitudinal arch as the toes extend during weight bearing, which in turn maintains the arch and stabilizes the foot. There is no elastic tissue in the plantar fascia, so all the work is performed via this tension mechanism.
Nurses are at high risk for developing plantar fasciitis due to our job responsibilities. The plantar fascia is composed of fibrous bands that insert at the heel (calcaneus) and connect to the toes (metatarsals). These bands provide support to the foot and in turn bear the weight of the body with ambulation and any weight bearing activity. The plantar fascia assists with shock absorption via a windlass mechanism. This refers to the fascia lengthening and increased tension on the medial longitudinal arch as the toes extend during weight bearing, which in turn maintains the arch and stabilizes the foot. There is no elastic tissue in the plantar fascia, so all the work is performed via this tension mechanism.
Common clinical symptoms include heel pain that is worse with the first step in the morning or after a longer period of inactivity, and similar heel pain after long periods of weight bearing (such as the end of a 12-hour shift). Onset is typically precipitated by recent increase in weight bearing (new exercise routine, etc.). On clinical exam, there is palpable tenderness along the plantar fascia, specifically, at the area of insertion at the calcaneus. The “windlass test” is also typically positive, (heel pain reproduced with passive dorsiflexion of toes). If you develop foot pain or heel pain, proper diagnosis is key.
Once diagnosed with plantar fasciitis, the cornerstones of therapy typically include conservative measures with a combination of stretching (both calf and plantar fascia), ice, rest, orthotics, strength exercises to stabilize the foot and ankle, and short-term non-steroidal anti-inflammatory drugs (NSAIDs). Physical therapy is also a recommended treatment. Let’s look at some of these treatment modalities.
Treatment
Home
- Rest
- Ice
- Try freezing a plastic water bottle (~ 16oz); once frozen, roll under your foot to ice the entire plantar fascia.
- Short term over-the-counter NSAIDS (for acute pain)
- Stretching
- Try rolling a tennis ball under the foot, massaging the plantar fascia.
- Perform stretches targeting the calf (gastrocnemius and soleus), hamstrings and Achilles.
- Over-the-counter orthotics (targeting distributing rear foot pressure)
- Heel support (heel cushioning to assist in shock absorption); silicone heel cups
- Medial arch support inserts
- Properly fitting shoes (Read Shoe Shopping – Put your best foot forward!)
- Motion control shoes
- Consider rotating shoes if working multiple days in a row.
- Limit time walking barefoot or in flip flops.
- Consider foot reflexology or massage by someone with experience treating plantar fasciitis.
Physical therapy
Typically includes:
- Proper assessment of foot posture and underlying structural deformities
- Manual therapy (massage, myofascial release) targeting mobilization of the plantar fascia, gastrocnemius and soleus myofascia, joint mobilization
- Stretching (calf, hamstring, posterior muscle groups)
- Anti-pronation taping
- Foot orthoses/custom options available
- Night splints (maintains a static stretch during sleep)
Orthopedist or Podiatrist
Potential treatment modalities:
- Corticosteroid injection
- Casting or controlled ankle motion (CAM) walker (boot); both designed to prevent weight bearing on heel and promote rest
- Extracorporeal shockwave therapy (ESWT); improves neovascularization of the area of pain by inducing microtrauma stimulating a healing process
- Surgery; plantar fascia release at the calcaneus (performed endoscopically)
Remember, as nurses we are lucky to work in a position that keeps us on our feet! From a health perspective, we do not face many of the health conditions related to prolonged sitting and sedentary desk jobs. There are industries dedicated to combat sedentary jobs by creating an “active office” – these interventions include standing desks, treadmill desks, and under-desk cycles, all focused on creating movement at work. This is already built into our jobs. I recently spoke with a cardiologist about the standing desk and she commented “they say sitting is the new smoking,” stressing the importance of movement and avoidance of prolonged sitting due to adverse health consequences. As nurses, we are ahead of the curve, most of our jobs are the opposite of a desk job. That said, we need to keep our feet healthy and feeling good for optimal job performance and comfort. The most effective way to prevent plantar fasciitis is to wear proper footwear at work, maintain a healthy weight, routinely stretch after a long shift, and if starting a new exercise or running program, build up to your goal rather than going all out on the first work-out. Lastly, pay attention to your feet, if you have pain, have it evaluated. In our busy work and home lives, let’s not forgot to give our feet some attention.
Do you have any tricks or tips you use personally to keep your feet healthy? Please share!
Reference:
Martin, R.L., Davenport, T.E., Reischl, S.F., McPoil, T.G., Matheson, J.W., Wukich, D.K., McDonough, C.M.; American Physical Therapy Association. (2014). Heel pain-plantar fasciitis: Revision 2014. Journal of Orthopaedic & Sports Physical Therapy, 44(11), A1-A33. https://doi.org:/ 10.2519/jospt.2014.0303