Homelessness and diabetes: nurses urged to help improve care

A nurse-led project has uncovered the challenges faced by people who are homeless and have diabetes and the ways that clinicians can improve care for this group.
The 15-month initiative gained insights from specialist inclusion health and diabetes nurses among other health professionals as well as people with lived experience.
“People experiencing homelessness with diabetes face multiple challenges”
Samantha Dorney-Smith
It found the experience of people experiencing both homelessness and diabetes to be “challenging, frightening and isolating with multiple barriers”.
Led by the charity Pathway in partnership with the Queen’s Nursing Institute (QNI) and others, the project included a survey with people working in inclusion health or diabetes services – 42% of whom were nurses.
The majority of participants – 57% – felt that diabetes care outcomes for homeless people were poor or very poor.
Two-thirds (66%) said, based on their professional experience, diabetes-related complications appeared to be more common in the homeless population than in the general population.
Asked about the barriers they face in providing care to this group, the most common answer (85%) was “patients’ complex needs” such as alcohol or drug use or mental health challenges.
This was followed by difficulty in contacting patients for follow-up (77%) and limited service resources (65%).

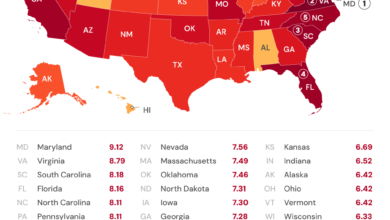
A graphic from the project
Meanwhile, almost all (91%) of the respondents said they had never received specialised training on providing diabetes care and support for people with complex needs.
This was despite the fact that 85% of participants had worked with homeless patients with diabetes in the last three months.
One survey participant said: “Patients struggle to access care due to chaotic lifestyles and lack of flexibility in the system.
“Professionals lack understanding of the challenges they face in the community and cannot adequately advocate for them or tailor their management to the patient’s needs.”
In terms of how care can be improved for people experiencing homelessness and diabetes, the top responses from health professionals included better collaborative working between mainstream healthcare, specialist healthcare and community organisations.
Flexible appointments and community outreach were also noted as useful strategies.
As part of the project, which was funded by the Burdett Trust for Nursing, feedback was also gained from people with personal experience of homelessness and diabetes.
They said the things that put them off engaging with health services included being ‘told off’ by clinicians; being advised to do things they would struggle to do as someone sleeping rough, such as storing medication safely or eating healthily; and simply being handed an information leaflet about their health condition.
On the other hand, they reported that explanations from nurses and receiving support in hostels made a “massive” positive difference to their experience of healthcare.
Informed by the findings of the project, a number of new resources have been created to help nurses and other health professionals working with this patient group.
The resources include a new homeless and inclusion health guidance document from the QNI.
There is also a free e-learning course and new tools to empower inclusion health and diabetes practitioners to audit their services and carry out quality improvement (QI) projects.

Samantha Dorney-Smith
The project was led by Samantha Dorney-Smith, a Queen’s Nurse and nursing fellow at Pathway.
She said: “People experiencing homelessness with diabetes face multiple challenges and are known to have very poor health outcomes.
“This project has brought together expert patients, specialist diabetes and inclusion health nurses and other allied practitioners to develop insights on how care can be improved.
“The resulting training resources are designed to support a whole range of professionals – from specialist diabetes practitioners all the way through to homelessness outreach workers.
“These resources are packed with tips to help improve care locally and to create better partnerships with patients and other services.”