‘Abysmal’ shortages of sickle cell nurses affecting care

A minimum ratio of specialist sickle cell nurses to patients is urgently needed to fix a long-standing “chronic underinvestment” in the specialism, a new report has said.
This new report, by the Sickle Cell Society, found a vicious circle of underfunding, lack of interest and poor exposure of sickle cell nursing to other nurses leading to gaps for people with the disease.
“We will continue to press for remedial action to be taken for sickle cell care”
John James
The charity, which represents the interests of people with sickle cell disease, today released The Difference Between Life and Death: An investigation into specialist sickle cell nursing workforce shortages.
This report forms a damning indictment of current funding and support for the condition, which predominantly affects people with African or Caribbean heritage.
The findings are based on evidence submitted by patients, families, specialist sickle cell nurses, consultant haematologists and other healthcare professionals.
Specifically, it called for more resources to train sickle cell specialist nurses as a way to plug an ever-widening gap between care for the disease and that provided for other, similar, conditions.
It made a series of recommendations to NHS England including minimum ratios for specialist nurses to patients, enhanced training and commissioning of specialist places and improvements to career progression for sickle cell nurses.
This, the Sickle Cell Society’s report said, would begin to break a cycle of a lack of interest in the nursing specialty.
The Difference Between Life and Death found that there was an “overwhelming consensus” among healthcare professionals, and the sickle cell community, that there is an insufficient number of specialist nurses to deliver proper care.
“The shortage of specialist sickle cell nurses means that patients’ care is frequently impacted by encountering nurses who do not have sufficient knowledge of sickle cell to deliver a good standard of care,” the report read.
“Specialist sickle cell nurses often do not have the time to engage with patients in the way that they would like, impacting their ability to properly explore problems patients are experiencing.
“This leads to some patients taking extreme measures, such as delaying or avoiding attending hospital due to their expectation of inadequate care.”
This investigation came after the publication of No One’s Listening, a report published by the organisation in 2021 which laid out gaps in care between sickle cell patients and other genetic conditions, such as cystic fibrosis.
No One’s Listening referenced racial discrimination that sickle cell patients experience when presenting at hospital, and spotlights several deaths including Tyrone Airey, whose case led to sweeping changes at the trust where he died.

Tyrone Airey, 46, died in hospital after being admitted in sickle cell crisis in 2021
The Difference Between Life and Death said underfunding and poor interest were problems which “reinforce each other”, adding: “Funding for specialist sickle cell nursing posts is seen as harder to secure than for other types of nursing positions, often connected to under-prioritisation of sickle cell among healthcare leaders and management.
“There is a perception among many nurses choosing a specialism that sickle cell care is an undesirable area to choose to work in.
“This can be due to nurses justifiably deciding that they do not wish to work in a particularly under-resourced area of healthcare.
“However, we were also told that sometimes prejudicial attitudes affect perceptions around the desirability of working with sickle cell patients.”
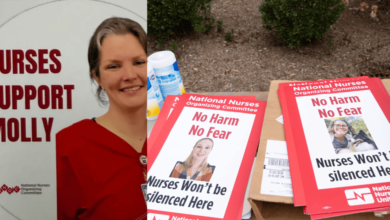
John James, chief executive of the Sickle Cell Society, said the findings of the surveys the charity carried out did not surprise him, and he hoped to see action from NHS trusts and integrated care boards (ICBs) within the next year to three years.
To help address the gaps in the nursing workforce for sickle cell patients, the report urged the NHS to invest more resources into it.
Currently, there is no mandated minimum specialist nurse to patient ratio for sickle cell. The Sickle Cell Society recommended a formal one be implemented by NHS England of 100 patients to one nurse at most.
The report further recommended NHS England undertakes a formal review of the workforce to find out where the needs are greatest.

John James at a Roald Dahl nurses event in London
According to the report, regional variations in the levels of care – including the numbers of sickle cell nurses – are still extreme and, on top of that, remedial actions taken so far have also varied hugely from area to area.
The report said NHS England needed to review how sickle cell nurses are commissioned, citing occasions where specialist nurses are not replaced when they leave, transfer or retire.
Mr James said that, for him, the most crucial recommendations were the 1:100 nurse-to-patient ratio and stamping out regional variations.
“One thing which emerged for me, which was important, was that unlike some other conditions like cystic fibrosis and Parkinson’s, there is no clear ratio for patients and nurses for sickle cell. It didn’t exist,” Mr James said.
“There needs to be one about how many patients a nurse can provide a good standard of care for, and we really want to get commissioners and ICBs to understand it.
“I just don’t know how [sickle cell nurses] do it, and I applaud their hard work.”
Mr James said it was crucial that ICBs, commissioners and the NHS itself took on board this ratio recommendation.
The Difference Between Life and Death heard from survey respondents that sickle cell care nurses were significantly overworked, even compared to other healthcare staff.
To combat this, and a lack of investment in technology to aid in sickle cell care, the report recommended a review into what NHS resources could be used to take the pressure off these specialist nurses, and for integrated care systems to fund “innovative medical technology” in the field.
Mr James continued: “There are problems across nursing, but for sickle cell there has been decades of underfunding.
“We are playing catchup; it’s not to say there aren’t big challenges for NHS systems, there is low morale at the moment – but I want to stress that sickle cell’s starting point is way back from those others, and the variation in nursing across the country is an important point.”
“Funding for specialist sickle cell nursing posts is seen as harder to secure than for other types of nursing positions”
Report
Mr James said that social and home care was something he wanted to raise the profile of, and described the “striking” gaps in community nursing that existed in sickle cell care.
He further said, in some areas, not only were things currently not improving but they were getting worse, with reports of sickle cell nurses not being replaced when one retired.
“The standard response [to our recommendations] from ICBs will be that they don’t have any money, which we understand,” he added.
“But that ignores the fact that when there was money, nothing was done, and that nothing was done about it for decades.
“We will continue to press for remedial action to be taken for sickle cell care, because it has been an abysmal starting level.
“Understaffing, care failings and neglect in the context of the country’s biggest genetic blood condition. If this were the case for something that affected the Anglo-Saxon population, I’m sure there would be a different discourse about it.”
The report recommends education providers, the Nursing and Midwifery Council (NMC) and the Royal College of Nursing (RCN) work with the Sickle Cell Society to make sure the disease “features adequately” in the nursing curriculum.
It also called for to national standards for nurses training in sickle cell, and more opportunities, including shadowing and secondment, for nurses interested in specialising.
Further, the Sickle Cell Society recommended a review of Agenda for Change banding for specialist sickle cell nurses and the establishment of clinical supervision support groups for these specialist nurses.