Fuel poverty scheme helping nurses to make ‘unbelievable difference’

A scheme that uses technology to identify and support respiratory patients who are at risk of fuel poverty has been transformative in just 12 months, according to nurses leading the initiative.
They said the population health technology had made an “unbelievable difference” to residents in Cheshire and Merseyside with chronic obstructive pulmonary disease (COPD) and facing fuel poverty.
“I’ve been a nurse since 1986, and we’ve never transformed lives like this”
Dianne Green
More than 1,000 patients have been identified and provided with assistance, including household support funds, pulse oximeters, new boilers, and access to wellbeing and rehabilitation teams.
Cheshire and Merseyside Health and Care Partnership forms part of the Cheshire and Merseyside Integrated Care System along with NHS Cheshire and Merseyside, the regional integrated care board.
The partnership said it had made significant progress since the launch of its fuel poverty programme, which uses population health technology to identify and support people facing fuel poverty.
The programme – called St Helens Warm Homes for Lungs – was first rolled out in February last year and uses digital dashboards to identify COPD patients that might benefit from more support.
Since then, more than 1,300 individuals at risk of developing serious health issues due to fuel poverty have been identified using Cheshire and Merseyside’s population health platform.
Patients have then been referred to council home improvement teams, which provided access to wellbeing and pulmonary rehabilitation, telehealth and for many, household support funds.
Payments totalling £106,000 have been made to patients, who have been reviewed by the specialist nursing team and offered a pulse oximeter and a warm home pack, including a vitamin D Voucher.
Those behind the project noted that the focus so far has been on patients with severe COPD residing in deprived areas and who are at high risk of admission due to cold and damp living conditions.
The partnership said it would now be expanding the COPD programme and rolling it out further across St Helens, Knowsley, and Warrington.
In addition, the next priority for Cheshire and Merseyside will be to use its fuel poverty dashboard, provided by Graphnet Health, to identify and support more vulnerable groups.
For example, in December, a Preschool Wheeze project was launched for children aged 0-4 with a respiratory wheeze.
It identifies and supports young children at risk of negative health implications, including asthma, due to cold homes.
Speaking on the programme so far, Dianne Green, a lead COPD nurse and service manager at Mersey and West Lancashire Teaching Hospitals NHS Trust, said she had seen a significant impact for patients.
“Through the fuel poverty dashboard, we’ve been able to identify patients in need and target them in a completely different way.
“As nurses, at the click of a button, we now have all the information that we need for those patients to truly help them,” said Ms Green.
“We can see whether they’ve been immunised, whether they are still smokers, whether they’re on the best treatment, and what quintile of poverty they are actually living in.
“That has helped us to prioritise and identify the people that are most in need,” she noted.
She added: “It is hard not to cry when speaking about the importance of this work, and how it has helped the patients that I support. It is truly proactive.
“I’ve been a nurse since 1986, and we’ve never transformed lives like this,” said Ms Green, who highlighted that the technology got round people’s traditional reluctance to ask for help.
“As a community nurse, we regularly go into patients houses but they never tell us that they can’t afford a light bulb upstairs, they never tell us that they’re really struggling to pay the bills….
“The difference that we’ve made by looking at them and their lives through different eyes, using this population health technology, is unbelievable,” she said.
Lucy Malcolm, senior digital transformation and clinical improvement manager for the partnership, added: “The technology provides the data that is needed.
“But it’s the people from health, social care, and other sectors, who have put their hands up to get involved; who are the heart of the programme, harnessing those insights to provide vital, life-improving support to Cheshire and Merseyside’s most vulnerable residents.”

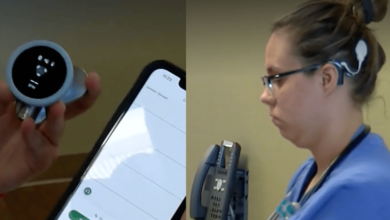
Dianne Green speaking about the programme at the 2024 Rewired conference