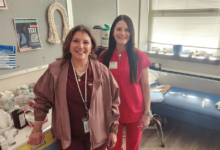
Government ‘must shift focus’ from hospital to community

Nurse leaders have welcomed a new report calling on the government to have greater focus on primary and community care but have warned that this would require investment in nursing “that we are not currently witnessing”.
The King’s Fund this week published a major report which has put forward the case for the health and care system in England to radically refocus and put primary and community care at its core, in order to be effective and sustainable.
“This solution is not about cutting vital hospital care, but significantly levelling up investment in essential community and primary care services”
Patricia Marquis
The think tank warned that failure to invest in primary and community health services was “one of the most significant and long-running policy failures of the past 30 years”.
Despite successive governments promising a vision where community care will be prioritised, it is still far from being achieved, the report warned.
It added that this was despite most interactions within the NHS taking place through primary and community services.
According to the report, government spending has been focused on the acute sector, with hospitals seeing a 27% funding growth since 2016-17, compared to just 14% for community trusts over the same period.
In their assessment for why this might be the case, researchers identified a “cycle of invisibility” for primary and community health and care services, noting that their value could be “hard to quantify and easy to overlook”.
Researchers also found that there were “hierarchies of care” that prioritised “crisis over long-term care” and that current challenges such as A&E wait times and care backlogs were higher on the agenda.
As such, the report called for future funding to be directed straight into a comprehensive plan to refocus the health and care system towards primary and community care.
Senior fellow at the King’s Fund and lead author of the report, Beccy Baird, said: “Like other countries, England needs to bend the curve on the predicted rise in demand for high-cost, reactive and hospital-based care.
“That means supporting people to take care of their health and wellbeing, intervening early and keeping people healthy at home for as long as possible, which can only be achieved by bolstering primary and community services.”
The King’s Fund came up with a list of specific actions that should be taken to make its vision a reality.
One of the key recommendations in the report was around bolstering the community and primary care workforce.
It comes as the NHS Long Term Workforce Plan has identified a need to grow this workforce faster than the acute workforce.
The plan, published in June last year, warned that there could be a shortage of 37,000 community nurses by 2036-37, compared to 6,500 in 2021-22.
According to the King’s Fund, based on these projections, the community and general practice workforce would need to grow faster over the next 10 years than previous decades.
The think tank estimated that 9,000 more community nurses would be needed by 2026-27.
The King’s Fund report called for more health and care leaders to be encouraged to pursue work in community settings.
As part of this, it noted the need for a collaborative approach by training providers and regulators to create “clear career paths” that can provide high-status roles in primary and community settings.
Meanwhile, training providers have also been told to explore how to “increase meaningful experience of primary and community care” to encourage students to choose these avenues as a career path. This could include compulsory placements in these settings, said the report.
Responding to the report, the Royal College of Nursing director for England, Patricia Marquis, said that patients and staff alike were experiencing “a drag towards the hospital” which did not always deliver appropriate or safe care.

Patricia Marquis
She said: “Care closer to home or in the home itself is both revolutionary and realistic.
“However, it requires a workforce investment that we are not currently witnessing.
“District nurses carry an unsafe and unreasonable caseload of patients and struggle to spend respectful or even safe amounts of time with people who need to see them.”
Meanwhile, Ms Marquis noted that primary care nurses, including those working in public health and prevention, needed a “clear incentive to join and stay working the community”.
She said: “They must be valued equally with nursing professionals in other sectors and specialties, getting at least the same pay, terms, and conditions as those employed by NHS hospitals.”
“As we approach the general election, all parties need to show they understand that this solution is not about cutting vital hospital care, but significantly levelling up investment in essential community and primary care services.”
Separately, the report urged for local health and care leaders to be granted greater flexibility to meet local needs, and to hold them to account for improving patient care rather than waiting lists.
In addition, it spotlighted a need for adult social care reform in England, if the ambition to have care closer to home is to be realised.

Martin Green
The chief executive of Care England, Professor Martin Green, welcomed this and said: “As we have repeatedly warned, acute pressures and the short-term nature of government funding cycles dominate health and care leaders’ capacity and resources.
“This means their scope to focus on long-term outcomes such as prevention is significantly hampered.
“We must strive for a system that is able to achieve meaningful outcomes, where people can have a seamless journey across health and social care.”
A Department of Health and Social Care spokesperson said: “This government wants to end short-term thinking and we are taking the long-term decisions that will mean everyone can access high-quality care that enables choice, control and independence.
“We commissioned the first ever NHS Long Term Workforce Plan to train, retain and reform the workforce, and put primary and community care on a sustainable footing.”