Mental health: nurses lay out demands for next government

Recognition of the unique nature of mental health nursing and action to tackle the underlying causes of poor mental health are among the changes that nurses want to see from the next government.
The proposals form the latest – and last – chapter of the Manifesto by Nurses, which Nursing Times has been building since October in anticipation of the next general election, the date for which has now been set at 4 July.
This final chapter outlines ideas from nursing professionals on how the political party that takes the helm can protect the mental health and wellbeing of the UK and futureproof mental health services.
A prominent theme among the responses was around the need to respect mental health nursing as a distinct specialty with different education needs to other nursing specialties, amid concerns that courses had become too generic.
More widely, nurses called for government policies that address the root causes of some mental health issues, such as poverty, as well as those that improve support for people who have the most severe mental health conditions.
There was also appetite for work to raise awareness with the public about mental health. More radical ideas included training up psychology graduates to provide therapy for some patients to help tackle waiting lists.
With the final chapter complete, Nursing Times will now collate all your ideas into a final manifesto that we will deliver to the main parties that are standing in the election.
Your mental health demands at a glance:
- More community mental health support
- More mental health nurses in primary care
- Improvements to mental health nursing education
- Action to address causes of poor mental health
- Routine mental health check-ups
- Public awareness campaigns about mental health
- Recognition of the uniqueness of mental health nursing
What you said:

Georgina Callard
Georgina Callard, mental health nurse in primary care, Queen’s Nurse and lead professional nurse advocate, Northamptonshire
Having mental health nurses in every general practice was the change Ms Callard wanted to see.
She said having more mental health nurses in primary care would support preventative work by helping people address their mental health concerns at an earlier stage.
“The demand is definitely there! I do this and have reduced referrals into secondary care, so it’s working,” said Ms Callard.
Alison Ruth Cross, specialist health visitor for perinatal and infant mental health, Blackpool Teaching Hospitals NHS Foundation Trust
“More money needs to be spent on mental health, but in the right way. Involve the people who are working in mental health and ask them what is needed,” said Ms Cross.

Alison Ruth Cross
She called for there to be “no postcode lottery” for good mental health care in the future.
In addition, she added: “More needs to be done to continue breaking down the stigma around mental health and the right people need to be in post to do this.”
Sally Davies and Yvonne Yelland, academics in Northamptonshire who both have more than 30 years’ experience in mental health nursing
The pair’s joint calls to action included one for “basic caring government policies” that ensured everyone had access to enough money to live on, somewhere to live and a decent job.
They also wanted to see the government assisting health professionals to educate the public about mental health and for more support for social prescribing via general practice.
In addition, they said steps needed to be taken to “ensure parity of esteem” between adult and mental health nursing – and for better recognition that the two fields are distinct and require different skills.

Erica Safar-Omoigui
Erica Safar-Omoigui, mental health practitioner, Plymouth
A “public enlightenment” campaign about mental health was something that Ms Safar-Omoigui believed would make a positive difference.
In addition, she wanted to see a “fairer career pathway” to allow all mental health nurses the opportunity to progress to advanced roles.
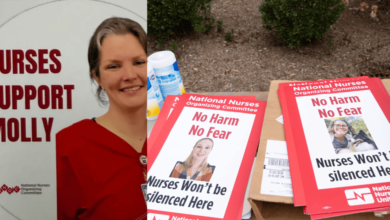
Stephanie Luff, clinical nurse specialist, London

Stephanie Luff
Ms Luff wanted to see the government taking further action to address the causes of poor mental health.
“We can’t fix mental health problems in reverse. They need to be fixed at the source – more social housing, more funding to schools, reasonable support for job seekers etc,” she said.
Dan Warrender, lecturer in mental health nursing, Abertay University, Dundee

Dan Warrender
“The future of mental health in the UK can be supported through developing well educated mental health nurses,” said Mr Warrender.
He warned that, at present, education standards were too generic and failed to “articulate a specific vision for what it means to be a mental health nurse”.
“An incoming government should prioritise emphasising the unique nature of mental health nursing, and improving the underpinning education of the workforce,” he added.
Jacqueline Parker, liaison and diversion nurse practitioner, North East London NHS Foundation Trust
Her demands included making mental health nursing a more “distinctive profession”, legally protecting the title of ‘nurse’, bringing back the nursing bursary, making sure all student nurses complete a mental health placement, and action being taken to support resilience in the population to “avoid labelling normal life struggles as illness”
Ed Freshwater, mental health nurse and postgraduate researcher, University of Leicester

Ed Freshwater
Mr Freshwater urged the next government to “wake up” to the “unbearable experience” of people with severe mental illnesses, such as schizophrenia and bipolar disorder.
“For years now – but more so since the pandemic – politicians, along with the public and media, have spoken about mental illness as if it’s only about mild-to-moderate anxiety, stress or low mood,” he said.
He claimed that people with severe mental illness had experienced “relentless attack from government” in the form of reduced benefits, deteriorating housing and fewer employment options – and called on the next government to change this.

Rachel Cadden
Rachel Cadden, newly registered mental health nurse, East Midlands
Her call was for routine mental health check-ups to be introduced for people at “high-risk ages and life stages”, and for investment in mental health drop-in centres.
Betty Scholes, senior lecturer in mental health nursing, University of the West of Scotland
“I would like recognition of the differences between mental wellbeing and mental ill health,” said Ms Scholes.
She said there should be non-medicalised pathways available for people to achieve mental wellbeing, as well as better investment in services for those with severe mental illnesses.
She also raised concerns that, due to a focus on “physical health and technical skills”, the current nursing curriculum was inadequate to prepare nurses for working with patients who were acutely mentally unwell.
“Greater recognition of the work of mental health nurses and investment in both the pre-registration preparation as a specialism and ongoing development of nurses… could redress this current imbalance,” said Ms Scholes.
Helen Bennett, nursing associate and student mental health nurse, Cygnet Health Care, Yorkshire

Helen Bennett
Ms Bennett said that more mental health support was needed in the community.
She suggested that the government could tackle waiting lists by making better use of people with degrees in psychology, who could be trained up to provide therapy for people with conditions such as personality disorders.
Michelle Orrell, mental health nurse, North West England
She urged the next government to “stop privatising and sending [the] most difficult mental health cases to private care”.

Michelle Orrell
In terms of mental health nursing, Ms Orrell said there needed to be improvements to pay, workloads, training, wellbeing support and workplace cultures.
Patricia Todd, retired mental health nurse, South East England

Patricia Todd
“The shortage of mental health nurses is a significant factor in the provision of good mental health care,” said Ms Todd.
She warned that these shortages meant newly registered mental health nurses were often “left to get on with the job, without the help and support they need” – and she called for this to change.
Mick McKeown, mental health nursing professor, North West England
Providing his insights for the next government, Professor McKeown said: “Mental health nursing can be one of the most rewarding jobs, with successful outcomes often depending on the skilled use of self within relational care processes.
“However, austerity cuts and workforce shortages put this under threat and services are becoming increasingly restrictive and coercive.”
He warned that a balance was needed in future to ensure that nurses still had enough time to provide direct and humane care in between record keeping and managing the use of technologies such as CCTV, body worn cameras and remote monitoring systems.
Brodie Andrew Paterson, consultant nurse psychotherapist, honorary senior lecturer, Scotland

Brodie Andrew Paterson
“Mental health nursing in the UK is in crisis,” warned Dr Paterson.
“Recruitment to courses is down. Practitioners are under enormous pressures, and they are emerging from increasingly generic training programs underequipped with the knowledge, skills and values to practice empathically, safely and effectively.”
He called for a “root and branch rewrite” of current standards for mental health nursing education, as well as workforce strategies that allowed nurses enough time to provide “relational practice” and reduced levels of burnout, compassion fatigue and moral injury.
Download a PDF of the mental health chapter below.