Neonatal lead warns nurses ‘really affected’ by Letby case

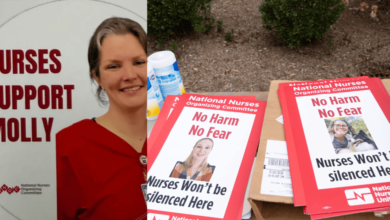
Neonatal nurses have been “really affected” by the Lucy Letby case, and need greater support from trust leaders going forwards, England’s lead neonatal nurse has said.
Louise Weaver-Lowe, who was appointed into the newly created role earlier this year, urged senior nurses to check in with staff on neonatal units, to see what additional support they can be given.
The comments came today as part of a panel on next steps for midwifery and neonatal care, at the chief nursing officer for England’s annual summit.
Ms Weaver-Lowe, who is a dual registered nurse and midwife, explained that the events surrounding Lucy Letby’s murder conviction had deeply impacted many in the profession.
Letby was sentenced to life in prison on 21 August for the murder of seven babies and the attempted murder of six others – crimes she committed while working as a neonatal nurse at the Countess of Chester Hospital NHS Foundation Trust.
Letby’s trial at Manchester Crown Court revealed how, between June 2015 and June 2016, the former nurse used various methods to harm the babies, including injecting air into the bloodstream, overfeeding with milk, physical assaults and poisoning with insulin.
“This extensive moral injury in neonatal services, I strongly felt that [after] the Letby outcome”
Tracey Brigstock
The government has confirmed that an inquiry will take place into the Letby case, which will be chaired by Lady Justice Thirlwall.
The inquiry will look at the experiences of the parents of Letby’s victims, the conduct of managers and staff working at the hospital, and the culture and governance procedures in the Countess of Chester and wider NHS.
Ms Weaver-Lowe said: “My thoughts are with those families that were affected by something that I think is unimaginable.
“And for neonatal [nurses] that was even more prominent [because] this was one of [their] own – so it really has affected them.”
Ms Weaver-Lowe explained that neonatal nurses already had to deal with complex births, where the outcome was sometimes not what parents “wanted or expected”.
“Their babies have been taken away, often very quickly after birth and that’s already traumatic,” she said.
“But now that dynamic has really shifted for parents to think [their] baby has been taken away by somebody [they] might not now be able to trust.
“And that really has felt hard for neonatal nurses.”
In a call to action, Ms Weaver-Lowe urged senior nurses at the conference to “think about your neonatal units”.
She explained that supporting staff through this period where neonatal care was in the spotlight would not only help nurses, but also families.
One programme she urged nurse leaders to consider implementing was the professional nurse advocate (PNA) role.
Nurses can become a PNA by completing a master’s level professional clinical leadership programme, delivered by universities, which provides them with skills to facilitate restorative supervision to their colleagues and teams.
Ms Weaver-Lowe argued that neonatal nurses could be “central” to bringing back confidence and trust on neonatal units across the country, by becoming PNAs.
“It’s the ability to [be able to recognise] that support is needed, and then to be able to give that restorative supervision to your colleagues,” she noted.
Kate Brintworth, the chief midwifery officer for England, also acknowledged the impact that the Letby case had had on staff working across maternity and neonatal services.
“It’s impossible to describe the horror that everyone felt around the events that have led us to the Thirlwall inquiry,” she said.
“I know that many of our neonatal colleagues have suffered great moral injury around those events.”
Tracey Brigstock, chief nursing officer at University Hospitals Coventry and Warwickshire NHS Trust, echoed this, and warned that the Letby case had had a significant impact on nurses within her organisation.
She said: “This extensive moral injury in neonatal services – I strongly felt that [after] the Letby outcome, walking in the neonatal services.
“[I was] walking the wards and being with the staff, talking to patients and service users [and] really getting a sense of what the unit felt like and what the culture felt like.”
Maternity services at University Hospitals Coventry and Warwickshire were this year given an ‘outstanding’ rating for leadership and a ‘good’ rating for safe by the Care Quality Commission (CQC)
It came as part of the watchdog’s national maternity programme, which aims to provide an up-to-date view of the quality of hospital maternity care across the country.
Ms Brigstock highlighted the ratings, and said they were “a bedrock to continue to improve upon”.
She noted that the trust had three maternity safety champions, of which she was one, and argued that they were “formidable” with their “relentless focus on maternity and neonatal services”.
Every two weeks the maternity safety champions sit down with maternity and neonatal staff to look at their maternity data together, Ms Brigstock explained.
“We reflect upon incidents that may have occurred and learning, and share that,” she said.
She argued that it was important for chief nurses to use the available data while also having a “soft focus” on the experiences of those on the units by having regular conversations with staff and service users.
Ms Brigstock added: “I think openness is really important, so we’ve worked really hard to do that.
“There’s always more work to do but the doors are open.
“There are fabulous maternity and neonatal teams out there.”