Nurses breaking bad news in mouldy and crumbling NHS wards

Crumbling NHS buildings are forcing nurses to break bad news to patients in rooms that are mouldy, have stains on the wall and holes in the ceiling.
A conference has heard testimonies from nursing staff about how inadequate investment in, and maintenance of, the NHS estate is impacting patient care across the UK.
“I think it’s really important that as nursing staff in hospitals that we have a safe place to work”
Sophie Ryder
The discussion took place during the Royal College of Nursing (RCN) Congress, being held in Newport this week.
Serena Bearpark, an intensive care nurse from the RCN North West London branch, told congress that the building she worked in was relatively new but that it had “a lot of leaks”.
“My colleagues noticed some water pouring out from one of the rooms quite quickly,” she explained.
“Then a bit later there was a stream of water coming from the ceiling above two patients bed spaces,” she said.
Ms Bearpark said that nurses and their colleagues had to work “very quickly” to get the patients safely moved out of the intensive care unit before “all the water came in and the ceilings collapsed”.
“Safe buildings should be a priority if we are to look after ourselves as well as our patients,” she added.
Elizabeth Morrison, a community mental health nurse, said her hospital only had half a roof for the last six months, which meant her team were unable to work from their offices.
“We do not have a room,” she said. “Because of this, I am having to discuss life changing diagnosis, such as dementia, with people in a room that smells of mould, has a hole in the ceiling and stains on the wall.”
Ms Morrison, who works in Scotland, noted that the Scottish Government had put its NHS building project on hold due to budget constraints.
She told the conference: “This is not good enough.
“This is not good for our patients, this is not good for our staff and it shows the regard nursing healthcare is held in the government.”
Meanwhile, Natalie Brooks described how her region, Norfolk, had four hospitals with reinforced autoclaved aerated concrete (RAAC).
Last year it was revealed that dozens of NHS sites in the country contained RAAC, a lightweight concrete containing air bubbles that was now reaching the end of its lifespan and, therefore, could crumble.
“We have four RAAC hospitals [and] one of them had over 234 props holding the building up,” she told delegates.
“In that hospital, my members have posters that say ‘did you see the ceiling move, if so report it now’.
“They are short staffed, they are working with patients in the corridor and now they’re looking at the ceiling – this has to stop.”
Sophie Ryder, a respiratory care nurse, highlighted the negative impact that failing buildings were having on patient health.
She explained that she had worked with multiple patients with aspergillosis, an infection caused by a type of mould, “from exposure to damp hospital buildings and asbestos”.
Ms Ryder said: “The majority of hospital buildings have asbestos in them – we are exposed to it every day.
“I think it’s really important that, as nursing staff in hospitals, we have a safe place to work [and] we are not exposed to occupational related diseases.”
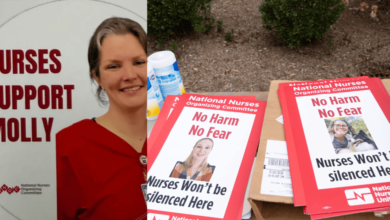
After hearing harrowing testimonies about the failing NHS estate and its impact on nurses’ ability to give care, RCN members decided to change the conference session from a discussion to a resolution.
Congress then unanimously voted to pass a resolution that asked RCN Council to lobby governments and care organisations to take action and maintain their estate properly.