Robert Francis: ‘rebuild’ trust between NHS and nurses

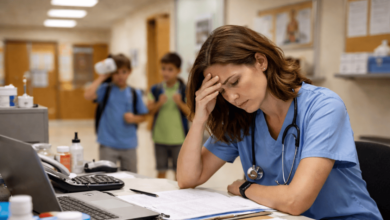
Too many nurses still don’t feel safe to raise concerns, Sir Robert Francis has warned.
Sir Robert, who authored a major review of the NHS’ speaking up culture in 2015, said there was a need to “rebuild” nurses’ trust in management and the health service following recurring scandals.
“It must sometimes feel that there is no end to the scandals”
Robert Francis
His comments came yesterday at the launch of the Florence Nightingale Foundation (FNF)’s health and care think tank.
The event, held in Reading, focused on the theme of speaking up, about which keynote speaker Sir Robert has been writing and speaking for around a decade.
He warned that if psychological safety and the workplace culture of the health service was not improved, whistleblowing would continue to be a luxury some staff feel they do not have access to.
“It must sometimes feel that there is no end to the scandals,” said Sir Robert, who led the investigation into care failings at the now-former Mid Staffordshire NHS Foundation Trust, and gave evidence this week to the public inquiry into serial killer nurse Lucy Letby.
He added: “Many nurses… are exhausted and rebuilding morale and trust will be one of our greatest challenges going forward.
“Unless we do that, speaking up will become more and more difficult.”
He aired his concern and frustration at a lack of improvement since Mid Staffs and the other inquiries, reports and reviews which have happened in the years since.
Sir Robert continued: “Over the years, we have had many reports, papers and guidance to tell us what good and safe practice looks like, what healthy culture looks like.
“What has struck me over the years is that these principles are generally accepted… but what happens then?
“Or what makes the change that is necessary to bring those good words into reality?”

Robert Francis
He pointed to the stubbornly high rates of staff who reported, via the most recent NHS Staff Survey, that they did not feel safe to raise concerns, and said there was still a long way to go to achieving the recommendations he and others have made about health service culture.
Reforms to culture, Sir Robert said, must also be accompanied by investment in the workforce, which he said was “undoubtedly” the best way to improve working conditions, and in turn patient care.
“Nurses need protection from having to work excessive hours, they need to have facilities – decent facilities – for taking breaks which they should take in reality, not just in theory.
“They should have places to rest, eat their lunch… support to get to work during antisocial hours.
“Why are these things we need to talk about?”
“Offering up inventive ideas or new ways of working. Sometimes, people don’t feel they can do that”
Becky Thomas
Sir Robert said the “freedom to speak up agenda” must be “applied in full”, adding that staff should not have to worry about isolation or being treated as “a maverick” for raising concerns.
His keynote speech was followed by a panel discussion on the same topic featuring King’s Fund senior fellow Professor Michael West; FNF chief executive Professor Greta Westwood; deputy director of safety and improvement at NHS England Jane Murkin; Mid Staffs whistleblower Helené Donnelly; Becky Thomas, leadership development facilitator at FNF; and senior nurses from University Hospital Southampton NHS Foundation Trust.
The panel discussed ways to improve the ability of nurses, and other healthcare staff, to speak up when they see something wrong at work.
Psychological safety emerged as one of the key themes from this panel, with Ms Thomas describing it as the “cornerstone” of nursing practice.
“You need to believe that you are safe, to take those interpersonal risks including speaking up on concerns, mistakes and even in positives,” she added.
“Offering up inventive ideas or new ways of working. Sometimes, people don’t feel they can do that.”
Professor West, similarly, said a “blame culture” in health when something goes wrong was preventing a psychologically safe environment from being created.
Ms Donnelly agreed, and also spoke about the need to better support, train and monitor managers in the NHS, pointing to the negative effect poor leadership could have on the speak up culture.
Echoing the aims of an ongoing project in which FNF is involved to create a national code of conduct for managers, Ms Donnelly said: “For me, the cultural change that’s needed across health and social care is around leadership, and leaders leading by example.
“I think though that leaders get a bit of a rough deal sometimes, because they are appointed into roles without the necessary support and skills and training that equip them to deal with some of this really difficult stuff, when people are speaking up about difficult issues.”